(Updated on 10 March 2022: To include replies from the polyclinics)
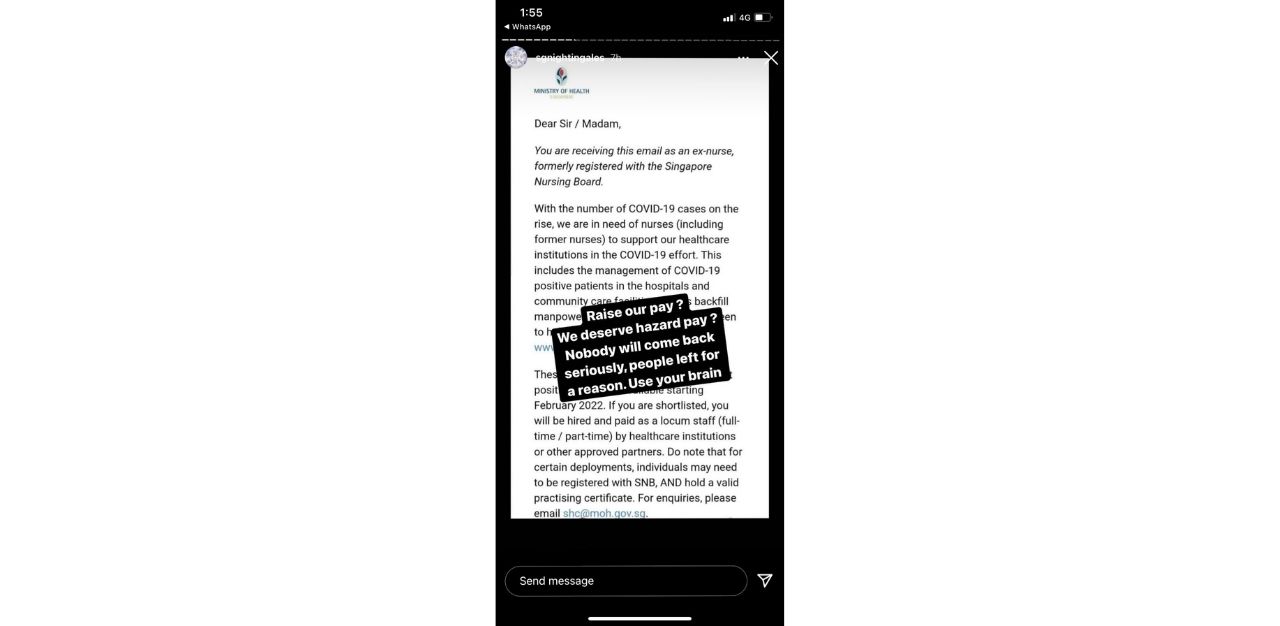
The Health Ministry (MOH) and public hospitals are working hard to redesign roles for nurses in a bid to retain staff and attract new ones. But on 15 February, Instagram advocates for nursing welfare, @sgnightingales, posted a sobering response.
Since the Covid-19 pandemic began, resignation rates among healthcare workers have been rising.
Senior Minister of State for Health Janil Puthucheary told Parliament in November 2021 that around 1,500 healthcare workers resigned in the first half of 2020 — compared with the already high resignation rates of 2,000 annually before the pandemic.
This number is even higher among foreign healthcare workers, who are unable to clear their accumulated leave to visit families back home. About 500 foreign doctors and nurses have resigned in the first half of 2020 — almost double the number in previous years.
“I think this has been an ongoing problem even before the pandemic. Covid just supersized everything,” says Ms Sheryl, a nurse who left the public sector about four years ago. She, like many others, has requested anonymity.
Mr Rex Ang, 23, a nurse who has been working at a private hospital for three months since graduating from nursing school, says the shortage in manpower applies to the private healthcare sector as well. “With Covid-19, the manpower crunch issue is quite real. Everyone is hoping to get by each shift, with every hospital having limited accommodations and high patient load within a very short period of time,” he says.
Ms Sheryl further shares that when she received the call to return to the public healthcare sector, she almost acceded to the request.
“Being a nurse, you feel that you have that sense of responsibility to help others and serve the country, as it is a nurse’s calling,” she says.
But there were ultimately many other factors that prevented her from doing so – no toilet breaks, no time for food until the shift ends, and the fear of bringing the virus home to her family. Ms Sheryl says that the mental health of nurses are also affected, with many suffering from pandemic fatigue, burnout, depression and anxiety.
“The manpower shortage just reflects that there is only so much that a nurse can tolerate. If not, we nurses would not choose to leave our posts at such a crucial period when our country needs us the most,” she says.
We are not really “coping well”
Inaccurate portrayals of the situation on the ground by mainstream media has likely exacerbated the mental health issues of the healthcare workers.
In January, the Straits Times reported that all hospitals in the island republic are “prepared for any potential surge in patients”.
“We have set aside existing beds that can potentially be converted to isolation beds for Covid-19 cases, as well as more holding facilities for suspect cases pending their results,” an NUHS spokesperson told the Straits Times.
This is, however, far from the truth on the ground, the nurses say.
“Maybe from an external point of view, it looks okay. But internally, a lot of healthcare workers are actually suffering,” says Mr Ang. “The number of nurses is going down, yet, the government is increasing our healthcare capacity. So we are definitely short of manpower.”
Ms Neo Yu Shan, who worked at Tan Tock Seng Hospital (TTSH ) for about 13 years as a community nurse before leaving last year, acknowledges that while upper management made the effort to check in with her, many other external factors still contributed to the stress she was facing at work.
“The shifts are just too long, and we are just physically and mentally tired. We always have to be on standby to get ready to help move Covid-19 patients to other departments, and it doesn’t help that MOH is announcing changes so frequently. We constantly have to adapt to them,” says Ms Neo, adding that the “messy management” contributed significant to her resignation, among other personal reasons.
“Be patient with us and play your part”
When asked how the situations can be improved in order for them to return, the answer was resoundingly about patience and social responsibility from the public.
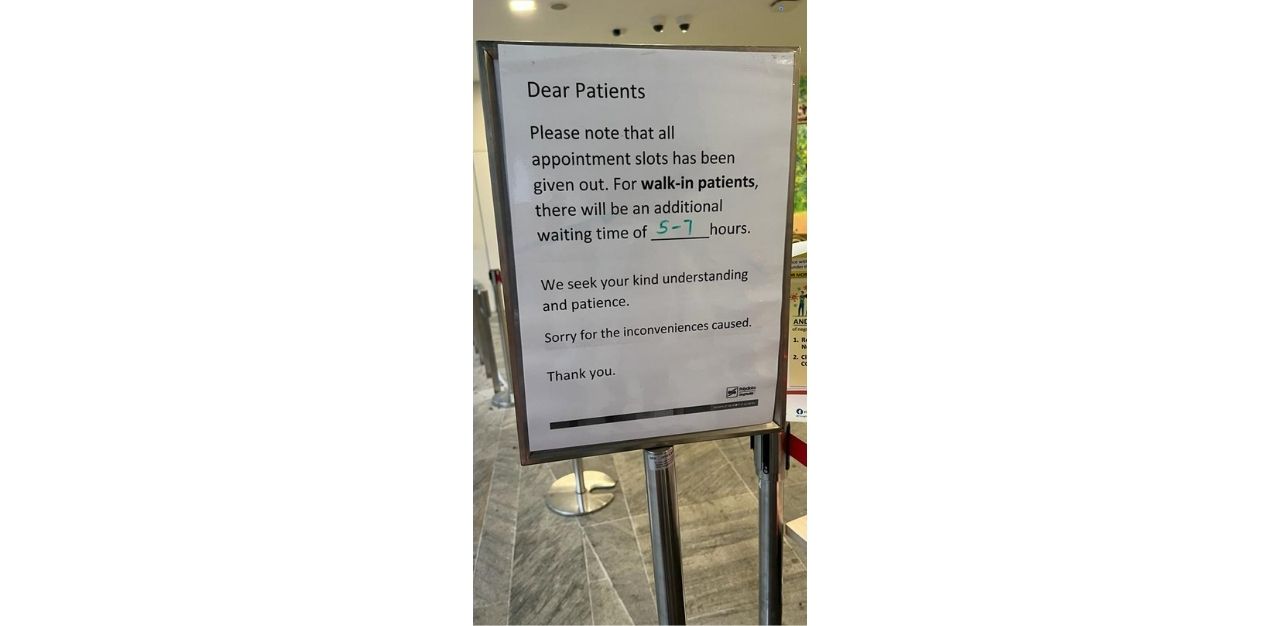
The long waiting periods at hospitals are not only frustrating for patients, but also healthcare workers, Ms Neo says.
“There are higher demands for shorter waiting times from the public [because of the perceived risks of Covid-19], and I visited a clinic recently, people who were waiting were becoming very angry and kept on pestering the nurses,” she says.
To ameliorate this, Mr Ang advises that the public can head to General Practitioner (GP) clinics instead of the emergency departments at the hospitals. “I think it’s understandable that parents are worried for their kids — they themselves are not doctors or nurses. Because of this, hospitals have been flooded with patients and this has caused a bit of unnecessary panic,” he says.
Additionally, he hopes that the public can understand that healthcare workers are also “giving 110 percent, in the middle of a pandemic, patient surge, and manpower issues”.
“Maybe if you ever feel like we are slow, I hope that you can try to understand instead of scolding us or cursing at us. This basic understanding can make our hospitals a much better place to work and be in,” he says.
In its email reply, SingHealth Polyclinics say the clinics are currently facing a patient surge due to the Covid-19 situation and longer waiting time for walk-in patients can be expected. The group also apologises for the inconvenience caused.
“Patients who have self-tested positive with mild or no symptoms, can make an appointment to undergo a self-administered Antigen Rapid Test (ART) under supervision at one of the Combined Test Centres (CTCs) or Quick Test Centres (QTCs) around the island if they require an official infection record,” its spokesperson says.
On the other hand, the spokesperson at the National University Polyclinics says the wait times for patients with an appointment across its polyclinics “have generally remained stable between November 2021 and February 2022.
“We have been strongly encouraging our patients to make their appointments via the OneNUHS app before visiting the polyclinic to minimise their waiting time and better manage their schedule. Digital ambassadors at the polyclinics teach our patients how to download and use the app, including scheduling appointments. With mobile registration, our patients are also able to register through the app before they arrive at the polyclinic, which helps in reducing their wait time for registration and overall wait time,” she says in an email reply.
Similar to the advice given by Singhealth, National University Polyclinics also says for those who have tested positive at home using ART kits but feel well to isolate at home for 72 hours. and that they need not see a doctor at the polyclinic and that a medical certificate is not required.
Join the conversations on TheHomeGround Asia’s Facebook and Instagram, and get the latest updates via Telegram.














