The Singapore tenet of ageing in place often means seniors are encouraged to age in their homes or the communities they live in, with aged care delivery system emphasising home and community based care.
This is nested within an overarching Action Plan for Successful Ageing and a policy shift toward a population health approach. This is seen by the government as consistent with the preferences of many older persons, aligned with filial piety and a means to optimise resources. This results in delivering value at lower cost by reducing unnecessary use of institutional care.
Social cultural anthropologist Thang Leng Leng says the concept of ageing in place has always been Asian as it “leverages on the Confucian values of filial piety and leans on family members for support of the elderly”.
“What Singapore needs is how to make the system and support better for the elderly to age in place. Singapore has a totally different system as children, who do not live with the elderly, still see themselves as caregivers. Also we cannot do without the support of foreign domestic help,” Dr Thang, who is also with the department of Japanese studies at the National University of Singapore (NUS), tells TheHomeGround Asia.
So, having Singaporeans age in place is in line with the Many Helping Hands Approach, a long established principle that calls for individuals, families, communities, civil society, the private sector, and government to all play a role in ensuring the well-being of the elderly.
“Kinship today is not limited to those within the family network since family structures are changing. Nurturing cross-generation relations within and beyond the family unit is important to get to know the seniors, to meet their aspirations as well as functional, cognitive and emotional needs,” Medical Director of Clinical Affairs at Tsao Foundation Raymond Leong says.
In a 2013 Forbes article, writer Benjamin Shobert, who is a current member of the Board of Advisors at the National Bureau of Asian Research, wrote that the Singapore government “needs to work much more quickly to allow its MediShield and Medisave programs to be used for home healthcare” and that the island state then faced “the unpleasant reality that its immigration policies prevent the inflow of the sort of caregiver workforce that will be necessary to take care of its ageing population”.
Community healthcare and Healthier SG strategy

Dr Leong says many Singaporeans grew up seeing their grandparents end up at long term care facilities “hence we think that the nursing home is the only and best place for an older person with multiple medical and social care issues”.
“Today there are more options to live, age and end in place. Daycare centres or home care are alternatives that older persons and their family members can consider if the senior is frail, requires help with daily activities of living, suffers from cognitive impairment, or needs social-psycho support,” he adds.
And that was the reasoning behind Healthier SG, the Government’s major healthcare initiative to focus on preventive care.
At the Committee of Supply 2022 in March, Health Minister Ong Ye Kung announced the strategy that champions the national shift towards a population health approach. He said it was “a journey that started more than ten years ago by previous Health Ministers, to focus on health, rather than cure”.
Adopted by many countries, population health aims to improve physical and mental health outcomes, promote wellbeing and reduce health inequalities across an entire population. It focuses on the wider determinants of health and activating people and empowering communities. It takes a life course approach with tailored strategies and segmented interventions.
Singaporeans’ health outcomes will be addressed from birth and throughout their life. And the population health approach will potentially tackle the challenges faced by Singapore’s healthcare system including a rapidly ageing population, increasing chronic disease burden and rising healthcare costs.
Mr Ong said the five key components of the Healthier SG strategy are:
- Mobilising Singapore’s network of family physicians, family doctors, as they can better detect early signs of problems timely and accurately;
- Healthier SG is a healthcare plan, so that the family doctor can assess overall health condition, conduct necessary health screenings, track your results, administer vaccinations if need be, and advise on adjustments in lifestyles to help with health goals;
- Singaporeans need community partnerships and support from agencies such as Health Promotion Board (HPB), Agency for Integrated Care (AIC), People’s Association (PA), SportSG, National Parks Board (NParks), and community partners that oversee various social services;
- A national Healthier SG enrolment programme that will be rolled out once the first three components are in place; and
- The necessary support structures which include manpower, finance and technology, to make Healthier SG work.
A White Paper was submitted to Parliament on 21 Sep and will be debated next month.
It has also been announced that from the second half of next year, Singapore residents aged 60 and above can enrol in the national programme to choose a family general practitioner (GP) to stick to and manage their health throughout the rest of their lives. To get their buy-in, the first onboarding health consultation for free.
Ageing in place, dying at home
With a growing preference among the elderly to age in place, staying put and spending their golden years in their existing homes, the government has launched Community Care Apartments (CCAs) for home buyers aged 65 and above. Apart from the affordable housing option, there are senior-friendly features and care services scaled according to care needs, giving options to elderly who require some care and support but are still able to and wish to live on their own.
The first lot of CCAs, located in Bukit Batok, went on sale in the February Build-to-order (BTO) exercise and the second pilot will be launched in Queenstown later this year. Dr Thang says it will be within the upcoming Health District in Queenstown, touted as Singapore’s first Health District to support residents’ well-being across their life stages, through tools such as better design and community programmes.

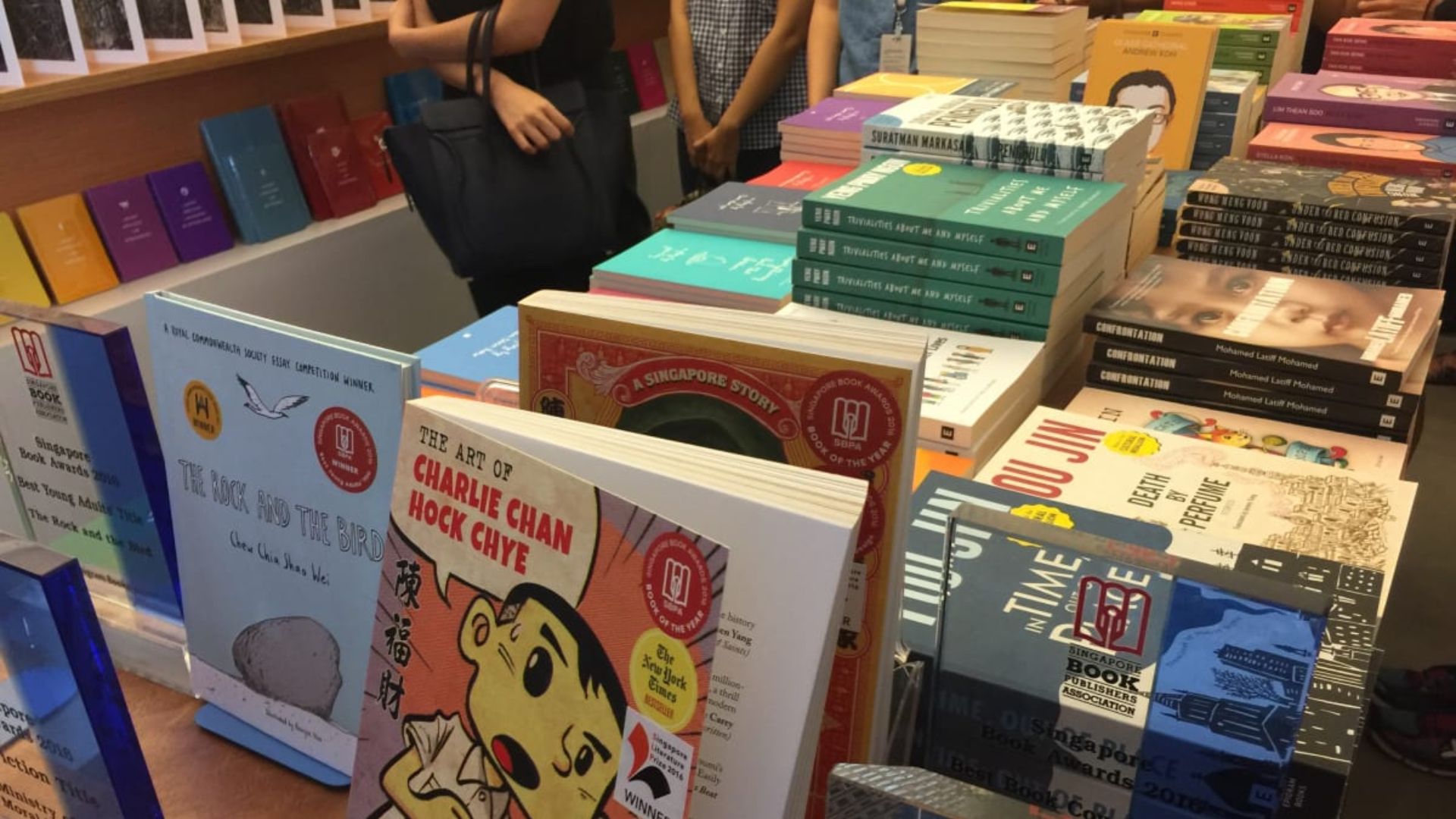
(Photo source: NUS News)
“It will help change mindsets and encourage the older residents to think about what they can do to be and feel useful, such as offering baby-sitting services, perhaps,” she says.
The Queenstown pilot is set to be a “model of a healthy and active community for all ages”, whose successful strategies may also be extended to more towns in future, said National Development Minister Desmond Lee.
Apart from all the infrastructures, Dr Thang says there is a need for long-term care insurance, “like the one in Japan”. Called Kaigo Hoken, it is a mutual assistance program in which the society supports those who need long-term care and those who are eligible to draw from the insurance services include those aged 65 years and older who need care because they are bed-ridden or suffering from dementia.
Such long-term care insurance covers between 70 and 90 per cent of the service cost and Dr Thang feels the Singapore Government could look into a similar long-term care insurance for the elderly to help them age in place. She believes existing insurance will not last the next 20 years for an elderly sick.
While many elderly want to age in place, they also want to die at home. A 2014 Lien Foundation survey found that while 77 per cent of Singaporeans hope to die at home, only 26 per cent manage to do so.
With 61 per cent still spending their final days in a hospital , Mr Ong said in June at his ministry’s workplan seminar that Singapore hopes to lower this figure to 51 per cent in five years (2027) by boosting support for palliative care.
The reasons preventing people from dying at home include family members not being receptive, hospital discharge process and protocols are challenging, and inadequate caregiver preparedness. So it is not surprising that MOH is working to raise awareness of and scale up palliative care capacity and better support caregivers at home. These changes will help reduce hospitalisation costs as as much as half the hospitalisation costs that people incur in their lifetime are racked up during the last three months of life.
Speaking from experience, Mr Ong said, “When my mother passed away, we had a palliative nurse who guided me along the way and really lowered the burden — not just in terms of time spent having to take care of her, but psychologically, what to expect.”
Dr Leong says, “Gerontological community nurses can influence the way older persons age well — through a good comprehensive assessment — and end well — palliative care. Often, they are advocates for the older persons too. They communicate well with older adults and their families, can assess geriatric needs, possess professional reporting skills critical for capturing concise and precise notes.”
“Seniors’ wish to age in place – including dying at home – can be met when more integration of medical and social services take place. For that to happen, the government, medical fraternity, clinicians, families and caregivers need to start recognising beyond the senior’s physical/functional needs but also their emotional and mental wellbeing,” he adds.
Embracing ageing: Alexandra Hospital’s effort to help its patients stay home, age in place
One hospital is helping its geriatric patients age in place. The patients at Alexandra Hospital (AH) are predominantly elderly, many of whom have multiple comorbidities. Appointments at different institutions, duplicate tests, unnecessary costs and inconvenience often result in care fragmentation and frustration for both the patients and their caregivers.

The hospital introduced its “seamless integrated care beyond discharge” programme to allow continuity of care, anchoring it in the safety and comfort of the home and community.
Resident physician Neeta Kesu Belani, who has been leading care consolidation at AH for about three years tells TheHomeGround Asia the elderly patients are cared for by a multidisciplinary team, made up of doctors, nurses, and allied healthcare professionals.
“They also have social issues and needs that require care management hence often a care manager or a social worker would be involved. This is crucial to support caregivers to ensure they continue caring for our elderly patients in the community; keeping them healthy and not requiring frequent hospital utilisation or admissions,” Dr Neeta says.
“This helps to keep all appointments under the same care team, identifying a principal doctor who leads a multidisciplinary team under the same hospital facility. This model is beneficial as it simplifies follow-up appointments of the patients, keeping them under the same roof, making it easy for caregivers to bring their loved ones for appointments,” she adds.
AH also has Alex Nurses in Community or AlexNic who care for patients in their homes.

“With one care team which communicates regularly with the patient’s caregiver and family, it helps us identify care gaps and challenges which the patient and family members are facing. This is crucial as medical care is never complete unless we approach them holistically,” Dr Neeta says.
AH Community Nurse Cassandra Kwek speaks English, Chinese and Malay and is often the one who trains domestic help and caregivers to care for the patients at home. Having worked as a nurse for 12 years, Ms Shu only joined the community nursing team in the last two.
“Community nursing is unique because we get to see how the patient is being cared for at home. We also work closely with the caregiver, assessing their work in taking care of the patient and correcting their errors on the spot instead of waiting for the patient to come into the hospital to realise the mistake,” she says.
Her colleague, assistant nurse clinician Sa’idah Jalani, adds that the rapport with the family helps “as we are able to assess and understand the situation at home and tell immediately if caregivers are coping well”.
Satellite geriatric services clinics in the community to help seniors age in place
For pre-frailty, AH launched its Geriatric Services Hub (GSH) in 2019 with direct access to specialised hospital-based services and resources. It has to date, received more than 500 referrals and enrolled about 250 patients, an over 50 per cent increase. About 2 in 5 patients took up its care coordination service.
There are currently three satellite geriatric services clinics set up by AH at Queenstown Polyclinic, and Lions Befrienders Senior Activity Centre at Clementi and Ghim Moh and are run by AH’s multidisciplinary medical team from the Healthy Ageing Programme.
“The Hub takes referral appointments by GPs or polyclinics for specialist geriatricians, nurses, pharmacists, physiotherapists, occupational therapists and care coordinators. The fees at these GSHs are lower than specialist clinics and are free for seniors living in rental blocks in Queenstown,” says Head of the Healthy Ageing Programme and GSH Santhosh Seetharaman.
Agreeing, the hospital’s CEO Jason Phua says, “Better patient-centred care can be delivered when age-related conditions are also managed along with the person’s multiple other medical conditions at the community level.”
For its effort, AH took the Healthcare Asia Award in 2021 for Patient Care Initiative of the Year.
RELATED: Ageing in place: Is it even possible in Singapore?
Join the conversations on TheHomeGround Asia’s Facebook and Instagram, and get the latest updates via Telegram.