Dr Brigitte Woo, research fellow at NUS Alice Lee Centre for Nursing Studies (NUS Nursing), grew up with a nurse for a mother who inspired her to pursue nursing instead of medicine.
“She was a visionary nursing leader,” Dr Woo says. “She had a grand vision of how we would one day see nurses in academia and politics.”
Today, the picture that Dr Woo’s mother had painted of nurses has become a reality. They are now researchers, clinicians, educators, and administrators.
“Nurses are now moving up the value chain. They are now more focused on care planning and management, rather than simple care delivery,” says Dr Chong Yap Seng, Obstetrician and Dean of NUS Yong Loo Lin School of Medicine.
Early this year in July 2021, Health Minister Ong Ye Kung announced that the Singaporean government hopes to have up to 700 Advanced Practice Nurses (APNs) in Singapore who are licensed to prescribe medication for patients by 2030.
“APNs are trained in the diagnosis and management of common acute and chronic medical conditions,” says Dr Zhou Wentao, an APN and Programme Director of the Master of Nursing Programme at NUS Nursing.
“We have APNs working in primary care, acute care, and community care settings, specialising in paediatrics, elderly care, cancer care, mental health care, and beyond,” she says.
While nurses in the past were purely trained based on direct clinical needs, healthcare professionals these days are being trained based on the needs of our ageing population.
“Doctors nowadays have to receive medical inputs not just from nurses but also from allied health professionals like physical therapists, pharmacists, and occupational therapists,” says Dr Woo.
Nurses critical in shift to community care
A key driver of this healthcare reform is our ageing population, with which chronic conditions are expected to rise. According to Dr Woo, current hospital-based, doctor-centric models of care will thus become unsustainable.
When patients with chronic conditions are sent for specialist consultations every time their symptoms act up, this not only chokes up limited hospital facilities but also racks up big bills for patients.
“We are looking to move stable patients with chronic illnesses that can be managed safely, from acute settings such as tertiary hospitals, into community facilities such as polyclinics,” she says. “These are situated within neighbourhood estates and are much more accessible and affordable for patients.”

By skilling up nurses, “one-stop-shop” clinics run by trained APNs can save patients trips to polyclinics and hospitals for their multiple conditions. Each patient saves up to three trips per year to the hospital.
The Covid-19 pandemic has helped catalyse this evolution of consultation modes, extending physical patient-doctor visits from six-month intervals to up to two years, according to Dr Zhou.
Consultation sessions at APNs are not only more affordable but also longer in duration as compared to physician consultations, which are known to be notoriously short. “This gives APNs a chance to build rapport with the patient, and properly educate the patient on how to manage their conditions on a day-to-day basis,” says Dr Woo.
Having conducted research on patients’ understanding and comfort levels with APNs, Dr Woo highlights that nurses are often able to establish a better rapport with patients, allowing them to provide holistic care, compared to doctors whose focus is more on diagnosis.
“I believe there is more intimate consultation time with the APNs, because the doctors need to see other patients. They might rush, but APNs are able to spare more time and we can discuss more issues,” says one patient in her study.
According to Dr Shefaly Shorey, Assistant Professor at NUS Nursing, when doctors ask patients if they have any further questions, they will often answer “no”, but turn around to ask the nurse what the doctor was saying. “In fact, this is such a cliché anecdote among nurses. It shows the trust that patients have in nurses,” she says.
APNs are also branching out in homecare services. For Dr Zhou, who targets patients with neurodegenerative diseases such as Parkinson’s, her key role is to prevent them from being admitted to the hospital, and instead educate family members on how to manage potential complications.
This care method saves families the hassle of moving elderly patients for regular appointments, which can be quite a struggle for both the patients and their families.
“A lot of lifestyle management wasn’t as well managed as it is now; there was more emphasis on acute care rather than chronic care,” says Dr Chong. “With more and more people getting chronic diseases like diabetes and hypertension, the role of nurses has become increasingly important.”
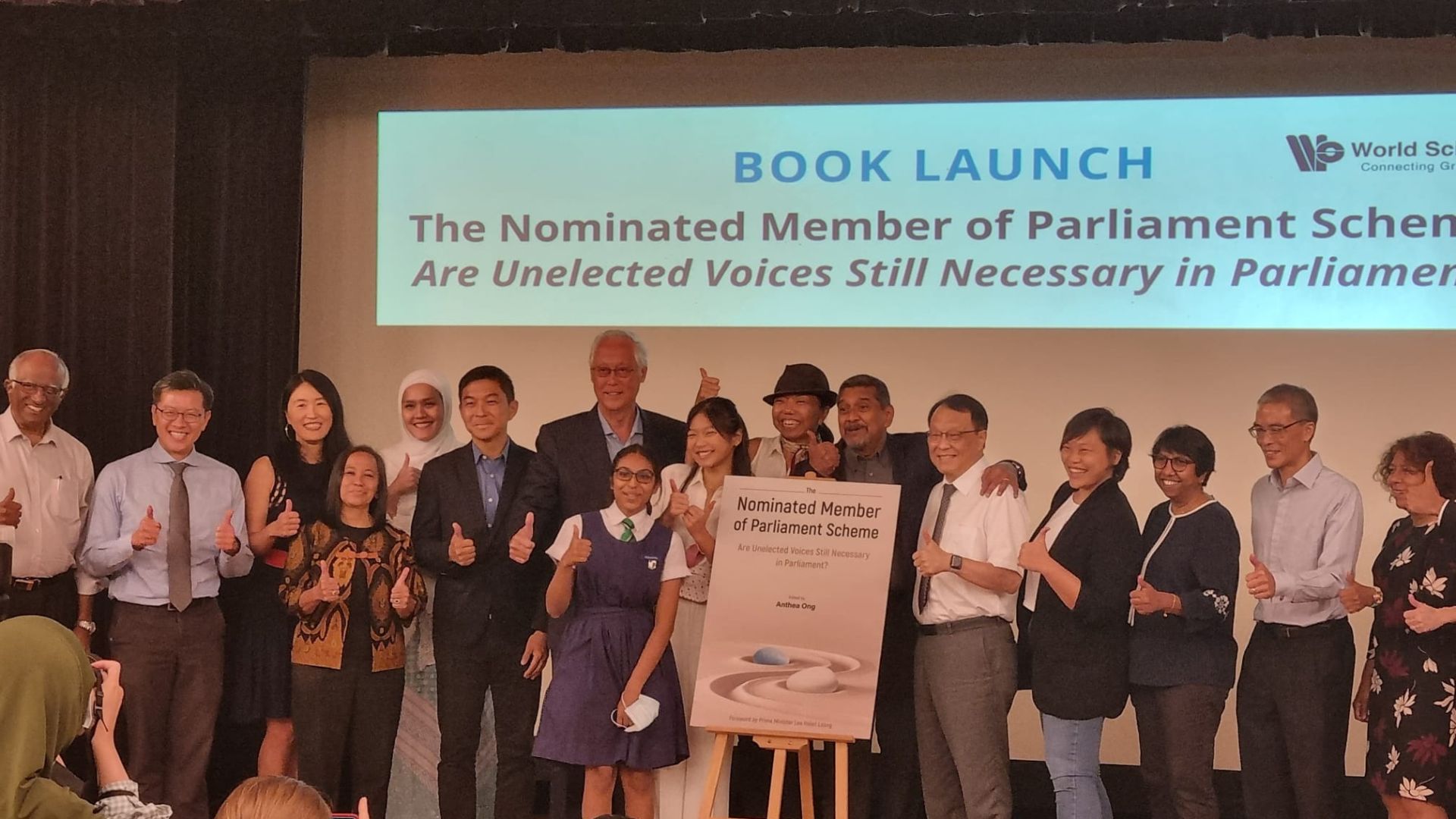
Nurses in academia and politics
While the relationship between nurses and doctors might have been more top-down in the distant past, Dr Shefaly believes that formal nursing education has been crucial to a more collaborative relationship.
“In the past, nurses were purely trained based on direct clinical needs, but now we are doing state-of-the-art work through evidence-based theoretical research,” she says.
“Doctors’ research focuses more on treatment and medication effectiveness, while for nurses, our research is more focused on holistic care and psychosocial modelling,” she adds, highlighting the rising need for nurses and doctors to combine their expertise and knowledge on equal and collaborative grounds.
Key surgical practices have been changed over time because of evidence-based research conducted by nurses.
While the option for nurses to pursue masters and doctoral degrees in Singapore is relatively recent — 10 to 15 years — it has been around in countries like the US and Australia for significantly longer.
Singapore’s recent evolution in nursing education has allowed nurses to surpass societal expectations of what nurses can do, with Dr Shefaly being a prime example.
“While nursing was a calling, I did feel limited when I graduated as I wasn’t familiar with many of the terms doctors would use when discussing patient cases, which is what motivated me to pursue a PhD in nursing research,” she says.
Dr Shefaly, whose specialisation is in midwifery, is one of the few researchers in the world working on fathers’ emotional needs, and whose papers are highly cited by medical professionals worldwide.
She shared that the practice of using alcohol to clean a newborn baby’s umbilical cord was discontinued due to nursing research, which showed that using cool boiled water is equally effective without having to expose the baby to alcohol at such a young age.
“We are crucial thinkers and problem solvers, and these changes only happened because nurses did not follow practices blindly just because they were written in the books,” she adds.

According to Dr Zhou, APNs’ diverse capabilities and rigorous training have additionally put nurses in a strategic position to work with other stakeholders to influence and shape Singapore’s healthcare system.
“A speaker at the International Congress of Nurses once mentioned that for any innovation, policy, or practice change to be effected successfully, one should always include a nurse on the team,” adds Dr Woo.
Most recently, the change in policy to allow nurses in the public healthcare sector to wear a tudung with their uniforms involved gathering the opinions of many nursing leaders.
Public perceptions are slowly changing
With the pandemic, Dr Chong believes that people are becoming increasingly aware of the importance of nurses in the healthcare system, and how the lack of nurses would be detrimental to society.
“We are now winning President’s awards, doing PhDs, and getting our papers published in academia. We will let our work speak for us,” adds Dr Shefaly.

Join the conversations on TheHomeGround Asia’s Facebook and Instagram, and get the latest updates via Telegram.